Digital technology and the prevention of suicide ideation.
Digital technology and the prevention of suicide ideation. Read More »

Narcolepsy is a sleep disorder caused by neurological changes that leads to difficulties regulating ones sleep-wake cycle. It can be seen in sudden sleep ‘attacks’ that can’t be controlled and cataplexy, which is when the individual suddenly loses muscle tone.
Diagnosis
Narcolepsy is diagnosed in the Diagnostic and Statistical manual of mental disorders (APA 2013) according to the following criteria:
The presence of at least one of the following:

Treatments
Narcolepsy can cause significant difficulties and dangers in everyday life and unfortunately there is no cure, but the are changes that can be made to help to alleviate symptoms. These include:
Lifestyle Changes:
Medication:
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
Anderson, T., Bandi, M., Bromley, K. D., Nino, M., & Terekhov, K. (2003). Narcolepsy.
M. Billiard, V. Pasquié-Magnetto, M. Heckman, B. Carlander, A. Besset, Z. Zachariev, J. F. Eliaou, A. Malafosse, Family Studies in Narcolepsy, Sleep, Volume 17, Issue suppl_8, December 1994, Pages S54–S59, https://doi.org/10.1093/sleep/17.suppl_8.S54
Mehta, R., Jiwanji, M., Singhal, R., Gillam, E., Lockwood, K., & Quarmley, M. (2021). The Social and Emotional Toll of Narcolepsy. Undergraduate Works.
There are so many options out there for you to choose from.
Your future is bright and clear. It may not seem it now but this storm will pass either way and you will shine.
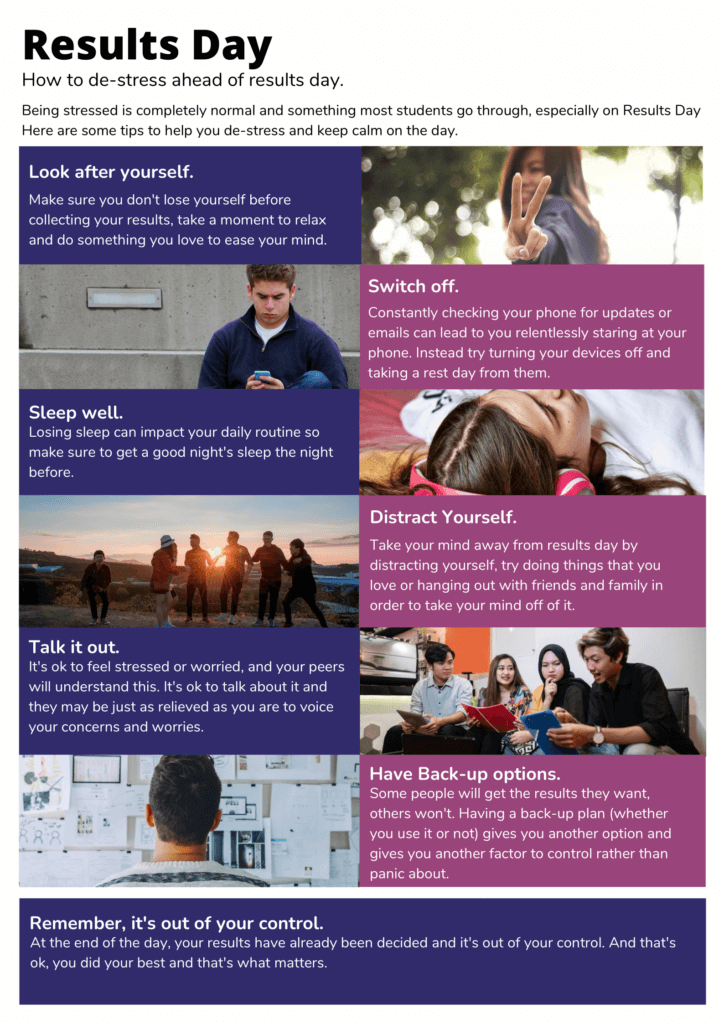
Remember you have done your best Read More »


What we eat doesn’t just affect our physical wellbeing but also impacts our mental health and overall mood. By taking this more holistic approach to wellbeing, we can lead healthier lifestyles and reduce the risk of physical and mental illness.

In general, a more ‘Mediterranean’ diet with whole foods, vegetables and fish is better for wellbeing compared to a more ‘Western’ diet of processed foods and red meats. However, food and wellbeing aren’t simply interrelated on the basis of what we eat but also when we eat. It is important to eat regularly as mood can dip when our blood sugar levels are low and eating regularly helps keep them at a stable level. It is important not to skip breakfast and eat smaller meals throughout the day and avoid foods that make your blood sugars rapidly increase, such as sugary soft drinks. Furthermore, it is key to stay hydrated as dehydration can reduce our memory ability and focus and water is also key in serotonin production which helps improve mood[1]
Understanding Eating Disorders:
While food is a source of pleasure for some, it can unfortunately be a source of anxiety and eating disorders can quite suddenly develop and become very harmful to our physical and mental wellbeing, Eating disorders such as anorexia and bulimia nervosa require professional intervention from a therapist and/or medication. Information on bulimia nervosa diagnosis and treatments can be seen in this article: https://www.linkedin.com/pulse/bulimia-nervosa-diagnosis-impacts-causes-treatments-/
References
Ocean, N., Howley, P., & Ensor, J. (2019). Lettuce be happy: A longitudinal UK study on the relationship between fruit and vegetable consumption and well-being. Social Science & Medicine, 222, 335-345.
Grosso, G., Galvano, F., Marventano, S., Malaguarnera, M., Bucolo, C., Drago, F., & Caraci, F. (2014). Omega-3 fatty acids and depression: scientific evidence and biological mechanisms. Oxidative medicine and cellular longevity, 2014.
Huntley, E. D., & Juliano, L. M. (2012). Caffeine Expectancy Questionnaire (CaffEQ): construction, psychometric properties, and associations with caffeine use, caffeine dependence, and other related variables. Psychological assessment, 24(3), 592.
Golomb, B. A., & Bui, A. K. (2015). A fat to forget: Trans fat consumption and memory. Plos one, 10(6), e0128129.
Golomb, B. A., Evans, M. A., White, H. L., & Dimsdale, J. E. (2012). Trans fat consumption and aggression. PLoS One, 7(3), e32175.
Gangwisch, J. E., Hale, L., Garcia, L., Malaspina, D., Opler, M. G., Payne, M. E., … & Lane, D. (2015). High glycemic index diet as a risk factor for depression: analyses from the Women’s Health Initiative. The American journal of clinical nutrition, 102(2), 454-463.
[1] Popova, N.K., Ivanova, L. N., Amstislavskaya, T. G., Melidi, N. N., Naumenko, K. S., Maslova, L. N., & Bulygina, V. V. (2001). Brain serotonin metabolism during water deprivation and hydration in rats. Neuroscience and Behavioral Physiology, 31(3), 327-332.
Physical and Mental Health Read More »
Body Dysmorphic Disorder (BDD) is an increasingly common anxiety disorder characterised by obsessive concerns with body image and perception which is prevalent more so in children and youth.


Causes and Risk Factors:
Treatments:
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
[1] Himanshu, A. K., Kaur, A., & Singla, G. (2020). Rising dysmorphia among adolescents: A cause for concern. Journal of family medicine and primary care, 9(2), 567.
[2] Monzani, B., Rijsdijk, F., Iervolino, A. C., Anson, M., Cherkas, L., & Mataix-Cols, D. (2012). Evidence for a genetic overlap between body dysmorphic concerns and obsessive-compulsive symptoms in an adult female community twin sample. American journal of medical genetics. Part B, Neuropsychiatric genetics : the official publication of the International Society of Psychiatric Genetics, 159B(4), 376–382. https://doi.org/10.1002/ajmg.b.32040
[3] Chandler, C. G., Grieve, F. G., Derryberry, W. P., & Pegg, P. O. (2009). Are anxiety and obsessive-compulsive symptoms related to muscle dysmorphia. International Journal of Men’s Health, 8(2), 143-154.
[4] Himanshu, A. K., Kaur, A., & Singla, G. (2020). Rising dysmorphia among adolescents: A cause for concern. Journal of family medicine and primary care, 9(2), 567.
[5] Vashi, N. A. (2016). Obsession with perfection: Body dysmorphia. Clinics in Dermatology, 34(6), 788-791.
“Challenges are gifts that force us to search for a new centre of gravity. Don’t fight them. Just find a new way to stand.”
Oprah Winfrey
A woman’s position in society is forever changing. With everything that has happened this month every woman across the UK is questioning safety, boundaries, relationships and gender identity. There will always be change and society is constantly evolving.
What is important now is to show kindness and respect to one another, whilst listening to the voice of all women and then focussing on how to share personal stories and let voices be heard. That is what will bring about true change not through violence but through compassion and listening.
International Women’s Day Read More »
What is Resilience?
In its simplest form, resilience can be defined as “the process of adapting well in the face of adversity, trauma, tragedy, threats or even significant sources of stress”. In essence, resilience is our ability to ‘bounce back’ when faced with challenges.

Why is resilience important for mental health?
Resilience is key to help us overcome adversity and maintain good mental health in the face of challenges that we will all face in our lifetime, such as bereavement or unemployment. Adversity can be extreme, for example the war in Ukraine and the chronic stress, anxiety and forced migration this is causing civilians. Adversity increases risk of developing a mental illness; however, research has found incidence of mental illness to be reduced in those who are resilient.
Why are some people more resilient than others?
While many individuals are mentally resistant to the repercussions of traumatic events, many people will develop chronic, debilitating mental disorders that reduce their quality of life and daily functioning. Why some people are more resilient than others is a complex question with several factors to consider, including:

Resilience and mental health Read More »
Christmas is always a joyful time of the year. Families enjoy decorating the whole house together, decorating the Christmas tree, exchanging gifts , baking and decorating Christmas cookies and also making Christmas cards. It’s a wonderful season that brings loved ones together and connected in a special way.
However, with the cost of living rising the festive season is looking rather expensive for families this year. Usually hundreds of pounds are spent on Christmas gifts and presents for our loved ones.
The cost of living crisis has had a huge impact on the lives of people within the economy. Families have had to resort to local food banks to help feed themselves and their families this season. Some people may be worries about how to pay their bills and have an enjoyable Christmas. This can have a negative impact on mental health and put people in real mental crisis. It is hard to get into the spirit of the season. Thats why more than ever it is important to be kind to one another.

With all this going on it seems nearly impossible to stay positive and have an enjoyable Christmas. However there is always a solution to every problem.
Reach out to a loved one or neighbour. Is there someone you see in your area that could do with some food and a smile? Christmas is meant to bring families together even distant ones. Reach out to friends or families and don’t be alone with your feelings and worries. Or do something in your community go to help at a local crisis centre or food bank. Please access organisations or support groups that are available 24/7 and are always willing to help. It may be a difficult time but you are never alone.
Remember to not overwork yourself this period. The bills are coming in and the kids need to be happy but this can lead to negative issues that cause harm to your body and I doubt your family would choose money over your wellbeing. Finally, spend time with your family or community. It’s Christmas after all .
Merry Christmas and have a blessed New Year.
Gambling addiction is a prevalent issue in the UK today and rates have increased across the pandemic, especially amongst younger people[1]. It has recently been recognised as a serious mental illness, as brain imaging shows the neural reward pathways that are formed, similar to those seen in alcohol and drug addiction[2]. The seriousness of the illness can also be seen in the disastrous effects it can have on one’s life, including relationship issues, job loss and bankruptcy, all of which increase suicide risk[3].
Diagnosing Gambling Addiction (DSM V) (APA, 2013)
The diagnostic and statistical manual for diseases (DSM V) diagnoses ‘gambling disorder’ according to whether the individual exhibits four (or more) of the following symptoms in a 12-month period:

Causes and Risk Factors:
Treatments
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
[1] Emond, A., Nairn, A., Collard, S., & Hollén, L. (2022). Gambling by young adults in the UK during COVID-19 lockdown. Journal of Gambling Studies, 38(1), 1-13.
[2] Murch, W. S., & Clark, L. (2016). Games in the brain: neural substrates of gambling addiction. The Neuroscientist, 22(5), 534-545.
[3] Andreeva, M., Audette-Chapdelaine, S., & Brodeur, M. (2022). Gambling-Related completed suicides: a scoping review. Addiction Research & Theory, 1-12.
[4] McComb, J. L., & Sabiston, C. M. (2010). Family influences on adolescent gambling behavior: A review of the literature. Journal of gambling studies, 26(4), 503-520.
[5] Newall, P. W. (2017). Behavioral complexity of British gambling advertising. Addiction Research & Theory, 25(6), 505-511.
[6] Mehroof, M., & Griffiths, M. D. (2010). Online gaming addiction: The role of sensation seeking, self-control, neuroticism, aggression, state anxiety, and trait anxiety. Cyberpsychology, behavior, and social networking, 13(3), 313-316.
[7] Castrén, S., Heiskanen, M., & Salonen, A. H. (2018). Trends in gambling participation and gambling severity among Finnish men and women: cross-sectional population surveys in 2007, 2010 and 2015. BMJ open, 8(8), e022129.
[8] Walther, B., Morgenstern, M., & Hanewinkel, R. (2012). Co-occurrence of addictive behaviours: personality factors related to substance use, gambling and computer gaming. European addiction research, 18(4), 167-174.
[9] Bodor, D., Ricijaš, N., & Filipcic, I. (2021). Treatment of gambling disorder: review of evidence-based aspects for best practice. Current opinion in psychiatry, 34(5), 508-513.
[10] Lupi, M., Martinotti, G., Acciavatti, T., Pettorruso, M., Brunetti, M., Santacroce, R., … & Di Giannantonio, M. (2014). Pharmacological treatments in gambling disorder: a qualitative review. BioMed research international, 2014.
Gambling during this season. Read More »
With all that is going on in the world at the moment many people are feeling anxiety and suffering from depression. Even though we try to get through the day without the stress caused by outside stressors, it can get increasingly difficult to find time for ourselves.
Anxiety is a feeling of unease, like a worry or fear that can show mildly or severe. It can present symptoms like a racing heart, shortness of breath and feeling shaky. It can also cause changes in behaviour like being overly cautious or avoiding things that trigger anxiety. It can cause you to not want to go outside, meet loved ones or generally interact with others.
Many people have different triggers but at the moment paying bills is a big cause of anxiety. People even dressed up as bills for Halloween.
There are ways to help us cope with anxiety. Trying to shift the focus helps to try and keep the mind in the present. You can try relaxation, mindfulness or breathing exercises and if they work for you then try and to do the exercises on a regular basis.
Keeping a diary might be a good practice for you as this allows you to understand your anxiety. You can write about how your feeling at different times and this can help you to identify the cause of your anxiety. From there you can build up a plan on how to tackle your anxiety.
Looking at the bigger picture could help you to see the situation your in, in a different light. It allows for you to stop and look at your problem rationally.
Try setting a specific time to look at what’s worrying you. This can help you to go through your concerns each day and can help you to focus on other things.