Feeling Less Stressed This Exam Season
As we head into exam season students may be feeling that the mounting pressure to do well is affecting their mental health. Taking exams can be a very stressful time, but there are things you can do to improve your mental health at all stages of the exam process.
Stress can be very overwhelming to deal with. Some symptoms include;
- tiredness
- feeling anxious or down
- feeling irritable or angry
- problems with sleep
- changes to eating habits
- worrying
- having bad thoughts about yourself
- not enjoying the things you love
- difficulties concentrating
- feeling physically unwell eg headache, stomach ache, sickness, fatigue.
Whilst some stress around exams is normal, experiencing these symptoms can interfere with your day to day life and make the process of taking exams more taxing than they should be.
The Exam Season
As the exam season begins, you may start to feel pressure to do well. This can come from a variety of places, from your teachers, parents, friends or even from yourself. There are a few techniques you can use to ease this pressure.
Firstly be kind to yourself, exams are tough and its important to remember that how well you do is only a small part of the many achievements you have accomplished.
Secondly, don’t compare yourself to other people. They may not look it, but they may be just as stressed as you. Everyone is coping in their own way.
Revision
Revising for exams can be stressful in itself. Make a revision timetable where you break work into reasonable chunks. Make sure to be realistic with your timetable, don’t schedule too much work in one day or you may burnout and feel bad about not achieving everything you wanted to do. Take regular breaks when revising to do things that make you happy, it is important to have a balance between work and play.
You can also look up the way you learn; visual, auditory, kinaesthetic and verbal are all different ways to retain information. Look into how you can use them in your revision methods.
If you work better with other people, join a study group. Tackling tough revision subjects together allows you to answer each others questions and fill in any knowledge gaps. This could help you feel more connected and less isolated as you study.
Before the Exam
There are many things you can do before the exam to ensure you are prepared. If you are struggling with a particular topic, talk to your teacher about it. They will be more than happy to help, they want to you to succeed.
You can also arrange access arrangements with your institution to make things easier for you, especially if you have special education needs or are neurodivergent, disabled, or deal with mental health issues. You could get extra time to complete an exam, assistive technology like a computer, or breaks during the exam. If you think access arrangements could help you, speak to your school to arrange them as early as possible as some need to be organised through an examining body.
Get organised the night before, pack your bag, know how you are getting to the exam, and make sure you have everything you need.
After the Exam
Well done you did it! You never have to think about Physics ever again!
Reward yourself by doing something you enjoy; hang out with friends, get a sweet treat or play video games. Let yourself rest and recharge before you continue revision for other topics.
Don’t compare your answers to other people. It may be tempting to ask others how they answered, but this only serves to make you question yourself and doubt your abilities.
Be kind to yourself. Remember exam results are not more important than your physical and mental wellbeing, and there is more to life than good grades.
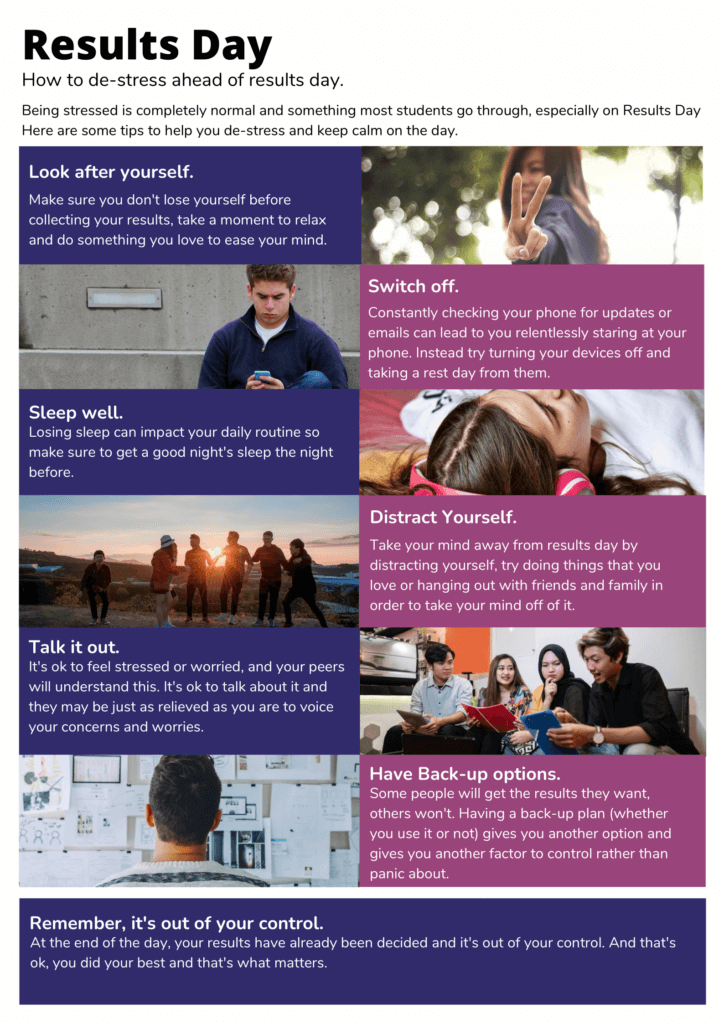
Results Day
If you don’t get the results you wanted remember exam results don’t define you and your worth is measured by a hundred other things. Make a list of things you want from life that aren’t exams and focus on life outside of education for a bit.
Explore your options, you could retake an exam, get it remarked or apply for special considerations. You could decide this qualification isn’t for you and switch subjects. You could rethink your career routes and choose something entirely different.
If you feel pressure to share your exam results remember you don’t owe anyone your results. It is absolutely fine not to share them.
Techniques to decrease stress
During this process you can use different techniques to decrease your stress and relax.
Try some relaxation techniques instead of cramming in last minute revision. You could do breathing or grounding exercises, or physical exercises like yoga or pilates.
Make sure you include self care in your routine, eat properly, drink plenty of water, sleep well and exercise regularly. Maintaining good self care provides a great baseline to improve your mental health.
Feeling Less Stressed This Exam Season Read More »